Diabetic retinopathy and diabetic macular edema
Diabetic retinopathy — vision-threatening damage to the retina of the eye caused by diabetes — is the leading cause of blindness among working-age Nigerians.
The good news: Diabetic retinopathy can often be prevented with early detection, proper management of your diabetes and routine eye exams performed by your eye doctor.
How does diabetes cause diabetic retinopathy?
Diabetes mellitus (DM) causes abnormal changes in the blood sugar (glucose) that your body ordinarily converts into energy to fuel different bodily functions.
Uncontrolled diabetes allows unusually high levels of blood sugar (hyperglycemia) to accumulate in blood vessels, causing damage that hampers or alters blood flow to your body’s organs — including your eyes.
Diabetes generally is classified as two types:
- Type 1 diabetes: Insulin is a natural hormone that helps regulate the levels of blood sugar needed to help “feed” your body. When you are diagnosed with Type 1 diabetes, you are considered insulin-dependent because you will need injections or other medications to supply the insulin your body is unable to produce on its own. When you don’t produce enough of your own insulin, your blood sugar is unregulated and levels are too high.
- Type 2 diabetes: When you are diagnosed with Type 2 diabetes, you are generally considered non-insulin-dependent or insulin-resistant. With this type of diabetes, you produce enough insulin but your body is unable to make proper use of it. Your body then compensates by producing even more insulin, which can cause an accompanying abnormal increase in blood sugar levels.
With both types of diabetes, abnormal spikes in blood sugar increase your risk of diabetic retinopathy.
Eye damage occurs when chronically high amounts of blood sugar begin to clog or damage blood vessels within the eye’s retina, which contains light-sensitive cells (photoreceptors) necessary for good vision.
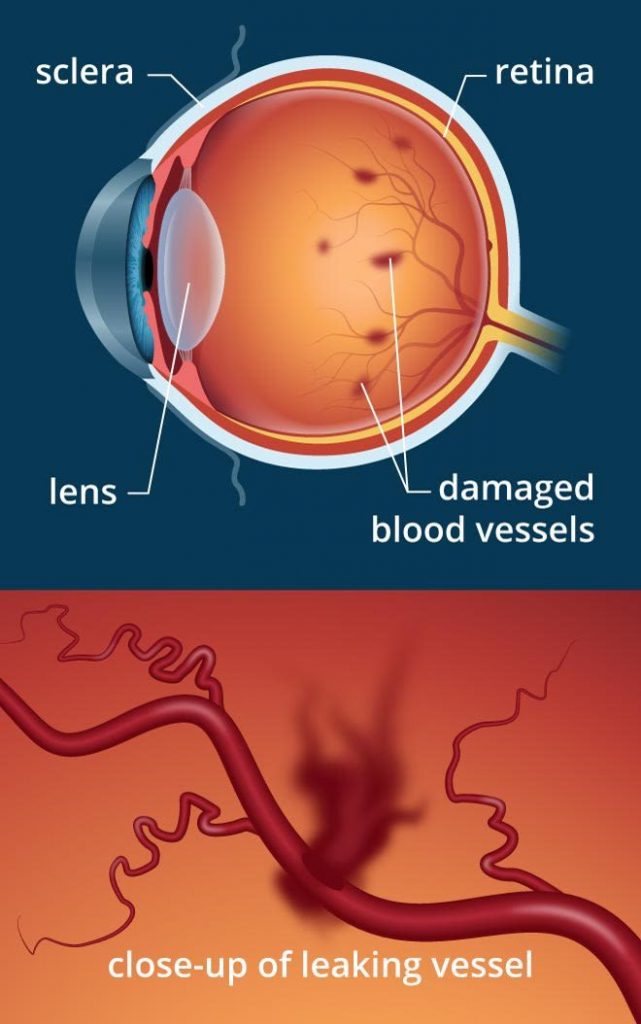
Among other problems, diabetes can damage blood vessels in the retina, causing them to leak blood into the posterior of the eye.
Diabetic retinopathy and diabetic macular edema symptoms
You may first notice diabetic retinopathy (DR) or other eye problems, including macular edema, related to diabetes if you experience symptoms such as:
- Fluctuating vision
- Eye floaters and spots
- Development of a shadow in your field of view
- Blurry and/or distorted vision
- Corneal abrasions
- Double vision
- Eye pain
- Near vision problems unrelated to presbyopia
- Cataracts
During an eye examination, your eye doctor will look for other signs of diabetic retinopathy and diabetic eye disease. Signs of eye damage found in the retina can include swelling, deposits and evidence of bleeding or leakage of fluids from blood vessels.
Your eye doctor will use a special camera or other imaging device to photograph the retina and look for telltale signs of diabetes-related damage. In some cases, they may refer you to a retinal specialist for additional testing and possible treatment.
For a definitive diagnosis, you may need to undergo a test called a fluorescein angiography. In this test, a dye is injected into your arm intravenously and gradually appears in the blood vessels of the retina, where it is illuminated to detect diabetes-related blood vessel changes and blood leakage in the retina.
One sometimes-overlooked symptom of diabetic eye disease is nerve damage (neuropathy) affecting ocular muscles that control eye movements. Symptoms can include involuntary eye movement (nystagmus) and double vision.
Types of diabetic eye disease
Once high blood sugar damages blood vessels in the retina, they can leak fluid or bleed. This causes the retina to swell and form deposits in early stages of diabetic retinopathy.
In later stages, leakage from blood vessels into the eye’s clear, jelly-like vitreous in the back of the eye can cause serious vision problems and eventually lead to blindness.
Clinically significant macular edema (CSME): This swelling of the macula is more commonly associated with Type 2 diabetes. Macular edema may cause reduced or distorted vision. Diabetic macular edema (DME) typically is classified in two ways:
- Focal, caused by other vascular abnormalities sometimes accompanied by leaky blood vessels.
- Diffuse, which describes dilated or swollen tiny blood vessels (capillaries) within the retina.
If you have CSME, you typically are advised to undergo laser photocoagulation treatment.
Non-proliferative diabetic retinopathy (NPDR): This early stage of DR — identified by deposits forming in the retina — can occur at any time after the onset of diabetes.
Often no visual symptoms are present, but examination of the retina can reveal tiny dot and blot hemorrhages known as microaneurysms, which are a type of out-pouching of tiny blood vessels.
In Type 1 diabetes, these early symptoms are rarely present earlier than three to four years after diagnosis. In Type 2 diabetes, NPDR can be present even upon diagnosis.
Proliferative diabetic retinopathy (PDR): Of the diabetic eye diseases, proliferative diabetic retinopathy has the greatest risk of visual loss.
The condition is characterized by these signs:
- Development of abnormal blood vessels (neovascularization) on or adjacent to the optic nerve and vitreous.
- Pre-retinal hemorrhage, which occurs in the vitreous humor or front of the retina.
- Decreased or blocked blood flow, with accompanying lack of oxygen needed for a healthy retina.
These abnormal blood vessels formed from neovascularization tend to break and bleed into the vitreous humor of the eye. Besides sudden vision loss, more permanent complications can include tractional retinal detachment and neovascular glaucoma.
Macular edema may occur separately from or in addition to NPDR or PDR.
You should be monitored regularly, but you typically won’t require laser treatment for diabetic eye disease until the condition is advanced.
Who gets diabetic retinopathy?
Beyond the presence of diabetes, how well your blood sugar is controlled is a major factor determining how likely you are to develop diabetic retinopathy with accompanying vision loss.
Uncontrolled high blood pressure (hypertension) has been associated with eye damage related to diabetes. Also, studies have shown a greater rate of progression of diabetic retinopathy in diabetic women when they become pregnant.
Of course, the longer you have diabetes, the more likely you are to experience vision loss.
CONTACT US AT PREMIUM OPTICALS AND EYE CLINIC FOR MORE INFORMATION.
Check this: Kemadrin

