Understanding dry eye syndrome
Dry eye syndrome is caused by a chronic lack of sufficient lubrication and moisture on the surface of the eye.
Consequences of dry eyes range from subtle but constant eye irritation to significant inflammation and even scarring of the front surface of the eye.
In addition to being called dry eye syndrome, dry eye disease, or simply “dry eye,” alternative medical terms used to describe dry eyes include:
- Keratitis sicca Generally used to describe dryness and inflammation of the cornea.
- Keratoconjunctivitis sicca Used to describe dry eye that affects both the cornea and the conjunctiva.
- Dysfunctional tear syndrome
Used to emphasize that inadequate quality of tears can be just as important as inadequate quantity.
Prevalence of dry eye
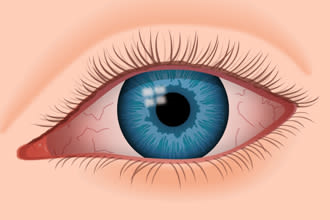
Dry eyes can become red and irritated, causing a feeling of scratchiness.
Dry eye syndrome — also called dry eye disease (DED) — is one of the most common eye conditions worldwide and a primary reason for visits to the optometry.
In a review published in the Journal of Global Health, researchers reported that studies have shown the prevalence of dry eyes ranges from 5 percent to as high as 50 percent in different populations across the world. (The researchers felt the large variation may be due to disparities in diagnostic criteria of different studies, unique characteristics of the investigated populations and other factors.)
Risk factors for dry eye syndrome included advanced age, female sex, and computer use.
Dry eye symptoms
Symptoms of dry eyes and dry eye syndrome include:
- Burning sensation
- Itchy eyes
- Aching sensations
- Heavy eyes
- Fatigued eyes
- Sore eyes
- Dryness sensation
- Red eyes
- Photophobia
- Blurred vision
Another common symptom is something called a foreign body sensation — the feeling that grit or some other object or material is “in” your eye.
As odd as it may sound, watery eyes can also be a symptom of dry eye syndrome, this is because dryness on the eye’s surface sometimes will over-stimulate production of the watery component of your tears as a protective mechanism. This “reflex tearing” does not stay on the eye long enough to correct the underlying dry eye condition.
In addition to these symptoms, dry eyes can cause inflammation and (sometimes permanent) damage to the surface of the eye. Dry eye syndrome also can affect the outcomes of LASIK and cataract surgery.
What causes dry eye syndrome?
An adequate and consistent layer of tears on the surface of the eye is essential to keep your eyes healthy, comfortable and seeing well.
Tears bathe the eye’s surface to keep it moist and wash away dust, debris and microorganisms that could damage the cornea and lead to an eye infection.
A normal tear film consists of three important components:
- An oily (lipid) component
- A watery (aqueous) component
- A mucous-like (mucin) component
Each component of the tear film serves a critical purpose. For example, tear lipids help keep the tear film from evaporating too quickly and increase lubrication, while mucin helps anchor and spread the tears across the surface of the eye.
Each tear component is produced by different glands on or near the eye:
- The oily component is produced by meibomian glands in the eyelids.
- The watery component is produced by lacrimal glands located behind the outer aspect of the upper eyelids.
- The mucin component is produced by goblet cells in the conjunctiva that covers the white of the eye (sclera).
A problem with any of these sources of tear film components can result in tear instability and dry eyes.
Dry eye categories
There are different categories of dry eyes, depending on which component is affected.
For example, if the meibomian glands don’t produce or secrete enough oil (meibum), the tear film may evaporate too quickly — a condition called “evaporative dry eye.”
The underlying condition — called meibomian gland dysfunction — is now recognised as a significant factor in many cases of dry eye syndrome.
In other cases, the primary cause of dry eye is a failure of the lacrimal glands to produce enough watery fluid (aqueous) to keep the eyes adequately moistened. This condition is called “aqueous deficiency dry eye.”
The specific type of dry eye often will determine the type of treatment your optometrist recommends to give you relief from your dry eye symptoms.
Factors associated with dry eye syndrome
A number of factors can increase your risk of dry eyes. These include:
Computer use
When working at a computer or using a smartphone or other portable digital device, we tend to blink less frequently and the blinks may not be full blinks , which leads to greater tear evaporation and increased risk of dry eye symptoms.
Contact lens wear
Though it can be difficult to determine the exact extent that contact lens wear contributes to dry eye problems, dry eye discomfort is a primary reason why people discontinue contact lens wear.
Ageing
Dry eye syndrome can occur at any age, but it becomes increasingly more common later in life, especially after age 50.
Menopause
Post-menopausal women are at greater risk of dry eyes than men of the same age.
Indoor environment
Air conditioning, ceiling fans and forced air heating systems all can decrease indoor humidity and/or hasten tear evaporation, causing dry eye symptoms.
Outdoor environment
Arid climates and dry or windy conditions increase dry eye risks.
Frequent flying
The air in the cabins of airplanes is extremely dry and can lead to dry eye problems, especially among frequent flyers.
Smoking
In addition to dry eyes, smoking has been linked to serious eye problems, including macular degeneration, cataracts and uveitis.
Health conditions
Certain systemic diseases — such as diabetes, thyroid-associated diseases, lupus, rheumatoid arthritis and Sjogren’s syndrome — contribute to dry eye problems.
Medications
Many prescription and nonprescription medicines — including antihistamines, antidepressants, certain blood pressure medications and birth control pills — increase the risk of dry eye symptoms.
Eyelid problems
Incomplete closure of the eyelids when blinking or sleeping — a condition called lagophthalmos, which can be caused by ageing or occur after cosmetic blepharoplasty or other causes — can cause severe dry eyes that can lead to a corneal ulcer if left untreated.
Also, LASIK and other corneal refractive surgery can sometimes cause dry eyes. In most cases, however, dry eye discomfort after LASIK is temporary and resolves within a few weeks of the procedure.
If you have dry eyes prior to LASIK, your optometrist may recommend a dry eye treatment program before your procedure to ensure the best possible LASIK results.
Dry eye tests
The only way to know for sure if you’ve got chronic dry eye syndrome is to have your optometrist perform one or more dry eye tests during an eye examination.
Symptoms alone are poor predictors of the presence and severity of dry eye disease. Symptoms can vary significantly from person to person, and may even be affected by personality type.
Some people with only minimal or mild dry eyes may feel their eyes are very bothersome, while others may have significant dry eye problems and not consider their symptoms significant enough to see an optometrist (or they may not experience dry eye symptoms at all).
Only a careful examination of your eyes by by an optometrist can reveal the presence and severity of dry eye syndrome and help your optometrist determine the best type of dry eye treatment to keep your eyes healthy, comfortable and seeing well.
Dry eye treatment and prevention
Thankfully, there are effective treatment options if you suffer from chronic dry eye.
In many cases, routine use of artificial tears and minor behavioural modifications (taking frequent breaks during computer use, for example) can significantly reduce dry eye symptoms.
In other cases, your optometrist might recommend prescription eye medications and in-practice procedures to help your body create and secrete more tears and to decrease eye irritation and inflammation.
CONTACT US AT PREMIUM OPTICALS AND EYE CLINIC FOR MORE INFORMATION.
You’ll be interested: Kemadrin

